Frailty and Vulnerability: Yes, you can lessen and even prevent Frailty
Written by Susan Moore
We’ve all met an older adult who we identify as frail. Some people use the words ‘frail’ and ‘vulnerable’ to describe older adults in general. Indeed, some older adults do become frail as they age but being frail doesn’t need to be a part of the normal aging process. Frailty and vulnerability can be mitigated and, ultimately, prevented.
How do you identify frailty? It is easier to identify what frailty is when we know how it is defined.
What is Frailty?
The Cambridge Dictionary defines frailty as “weakness and lack of health or strength” . Healthcare literature provides highly detailed descriptions of frailty to recognize, diagnose and treat Frailty Syndrome. Zachary Palace and Jennifer Flood-Sukhdeo describe Frailty Syndrome as the development of multiple age-related musculoskeletal changes leading to physical weakness, injury and illness . In other words, Frailty Syndrome occurs in an older adult who has lost muscle and bone strength, and who is more prone to falls, fractures and vulnerability to increasingly complex illness and injury. The bad news is – we are all at risk of frailty. As we age, our bone density, muscle strength and stamina start to change. This degeneration is a normal part of the aging process. However, the good news is that frailty does not have to be a part of aging. It can be prevented and at the very least, its impact can be lessened.
Diagnosis
In general, frailty is diagnosed by a physician based on a number of indicators including physical strength, bone density and nutrition. Once someone is diagnosed with Frailty Syndrome, physicians will rate the degree of frailty based on someone’s ability to carry out “instrumental and non-instrumental activities of daily living” . It is important for physicians to identify frailty indicators as early as possible so that patients have the opportunity to change or adapt their behaviours. An early diagnosis is the key to reversing the symptoms of frailty. As with most disease, the longer it takes for symptoms to be identified and a diagnosis made, the more vulnerable the patient becomes to increased risks associated with treatment of illness and injury.
Causes and Prevention of Frailty
When it comes to frailty, an ounce of prevention is worth a pound of cure.
According to Humankinetics.com , the causes of frailty include:
- A medical condition
- A loss of one or more senses
- A chronic disorder
- A chronic disorder along with a new medical diagnosis
- Adverse changes in the musculoskeletal system
- Psychological issues
- Sarcopenia (loss of muscle mass)
- Very old age
- Nutritional imbalances
- Intellectual disabilities
- Physical inactivity
The British Geriatrics Society identifies the causes of frailty as: inactivity, low protein diet, insufficient vitamin D, smoking and obesity. Some of the causes are directly linked to illness and injury (dementia, broken bones, flu) and others are based on personal habits and behaviours.
We have the power to change our behaviours and lessen the risk of becoming frail.
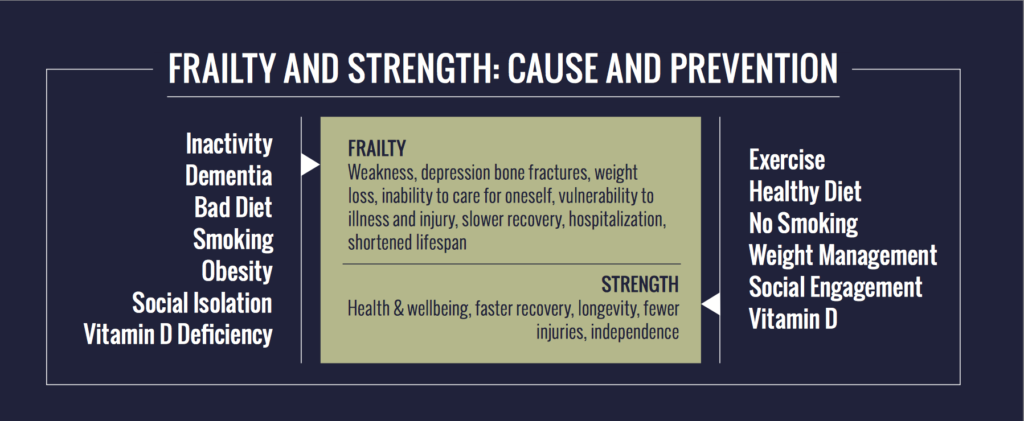
Based on the identified causes of frailty, we know that some identified factors can’t be avoided. Dementia, intellectual disabilities and other chronic conditions increase older adults’ vulnerability to frailty. The reality is that frailty can be avoided or minimized by developing behaviours that will keep us physically, mentally and emotionally healthy.
The key to not developing frailty is early detection. Visit your doctor if you notice changes in your energy or physical strength. Get off the sofa and walk around the seawall, lift weights, join an exercise class. Stop smoking. Eat smaller meals more often to maintain a healthy weight. Engage with your community. All of these actions can lower the severity of frailty and increase the chances for recovery.
Many older adults face challenges when it comes to staying strong and healthy as they age. Socioeconomic factors including poverty, isolation and geography can be barriers. However, barriers and a predisposition to developing frailty are not absolute and can be addressed with low or no financial burden. There are seniors’ centers, neighbourhood houses and community centres throughout Metro Vancouver, many of which provide healthy meals, physical activity, lifelong learning and an opportunity to socialize. Older adults who are unable to leave their homes, can also be active and engaged through programs such as Friendly Visiting, Peer Support, Meals-on-Wheels and grocery delivery. The staff and volunteers working in community agencies can often provide you with information and referral to agencies providing more complex care when needed.
If you or someone you know has been described as frail by peers, family or friends, or if there has been a diagnosis of frailty syndrome, you can do something(s) about it:
- Medical conditions – follow your physicians’ treatment plans including medications and therapies
- Chronic disorders (i.e. arthritis, hypothyroidism and high cholesterol) – stay physically active, rest when needed, follow a healthy diet
- Adverse changes in the musculoskeletal system – lift weights, sweat, drink water and stay active
- Psychological issues – call a friend, engage with your local community, ask for help when needed, volunteer to help others
- Nutritional imbalances – eat a well-balanced diet and take your vitamins as directed by your healthcare professional
- Physical inactivity – dance, swim, join a walking group, plant a garden or volunteer to help someone with theirs.
Frailty does not need to be inevitable. If you are concerned about your predisposition to developing frailty syndrome, speak with your doctor, a friend or family members. If you are concerned about someone else, contact the seniors’ centres in your community for information and referral to a professional who can advise you on how to help.

Susan Moore